why does the brain confuse nicotine for acetylcholine
Nicotine, a chemical found predominantly in tobacco products, is often associated with addiction and smoking-related health issues. But why does the brain confuse nicotine for acetylcholine, a crucial neurotransmitter? This question lies at the heart of understanding nicotine addiction and its profound impact on the human brain and body. The confusion occurs because nicotine mimics the structure and function of acetylcholine, binding to the same receptors and altering normal brain function. This article delves into the specifics of this interaction, explores the physiological consequences, and discusses the broader implications for health and addiction.

What Are Nicotine and Acetylcholine?
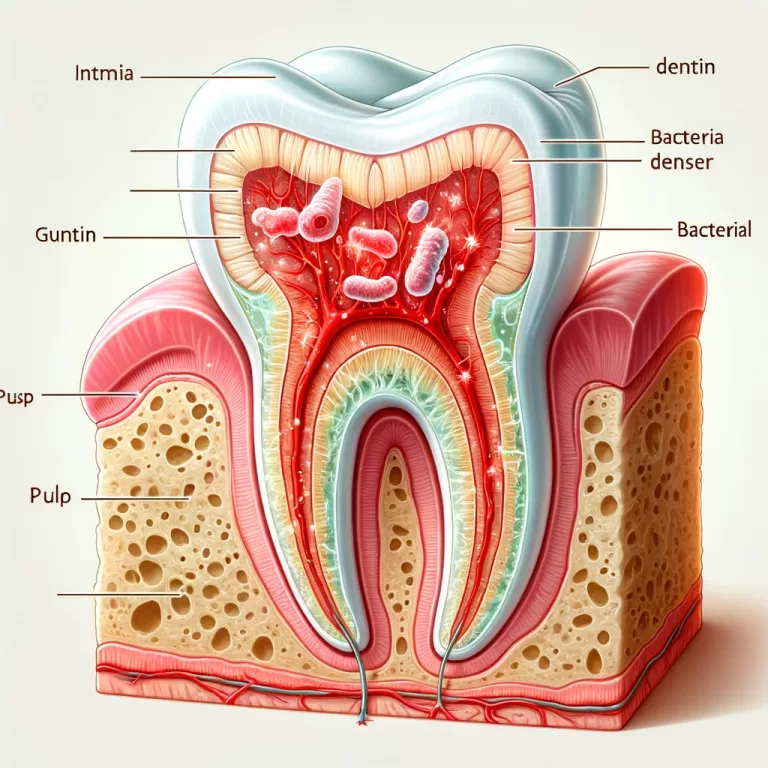
Acetylcholine is a neurotransmitter that plays a critical role in the brain and peripheral nervous system. It is involved in various functions, including muscle contraction, heart rate regulation, memory, and attention. Acetylcholine binds to nicotinic acetylcholine receptors (nAChRs) located on neurons, which are ion channels that allow the flow of ions into the neuron, facilitating neurotransmission.
Nicotine, on the other hand, is a stimulant found in tobacco and other plants. When inhaled or ingested, nicotine quickly crosses the blood-brain barrier and binds to nAChRs, imitating acetylcholine. However, unlike acetylcholine, nicotine is not naturally regulated by the body, leading to overstimulation of the receptors and a cascade of neurochemical effects.
How Does Nicotine Mimic Acetylcholine?
The molecular structures of nicotine and acetylcholine share similarities that allow nicotine to fit into acetylcholine’s receptor sites. Nicotine has a tertiary nitrogen atom that closely resembles acetylcholine’s quaternary nitrogen, enabling nicotine to bind effectively to nAChRs. This binding triggers the same response as acetylcholine: the opening of ion channels and the subsequent flow of calcium, sodium, and potassium ions into the neuron.
However, the effect of nicotine binding is not as benign or well-regulated as acetylcholine’s. Nicotine’s binding is stronger and lasts longer, leading to prolonged activation of nAChRs. This persistent activation disrupts normal neurotransmitter regulation, leading to increased dopamine release and, over time, altering the brain’s reward system.
Why Does the Brain Confuse Nicotine for Acetylcholine?
The confusion between nicotine and acetylcholine arises due to their similar shapes and functional groups, which allow nicotine to effectively “trick” the brain’s receptors. This mimicry does not mean that nicotine acts exactly like acetylcholine in every respect; rather, it hijacks the acetylcholine pathway, leading to unnatural and often harmful consequences.
One of the most notable effects is on the brain’s reward system. Nicotine’s ability to stimulate the release of dopamine—a neurotransmitter associated with pleasure and reward—leads to feelings of relaxation and euphoria. Over time, the brain becomes dependent on nicotine to maintain these elevated dopamine levels, contributing to addiction.
The Physiological Impact of Nicotine Binding to nAChRs
- Dopamine Release and Addiction: When nicotine binds to nAChRs, it leads to the release of dopamine in the nucleus accumbens, a key area involved in the brain’s reward circuitry. This release creates a sense of pleasure and reinforces behaviors associated with nicotine use. With repeated exposure, the brain becomes conditioned to seek nicotine to stimulate dopamine release, perpetuating addiction.
- Cognitive Enhancement and Decline: Initially, nicotine can enhance cognitive functions such as attention, learning, and memory due to the stimulation of nAChRs in the brain. This has led to some research into nicotine’s potential therapeutic uses in conditions like Alzheimer’s disease. However, long-term use results in desensitization and downregulation of these receptors, leading to cognitive decline and impaired neurological function.
- Autonomic Nervous System Effects: Nicotine’s action on nAChRs in the autonomic nervous system affects various bodily functions, including heart rate, blood pressure, and gastrointestinal activity. For example, nicotine stimulation can increase heart rate and blood pressure by activating receptors in the adrenal medulla, leading to the release of adrenaline.
- Impact on Mood and Stress: Nicotine influences the release of other neurotransmitters, such as serotonin and norepinephrine, which are involved in mood regulation. While some users may feel a reduction in stress or anxiety with nicotine use, these effects are often temporary and can lead to increased anxiety and mood swings when the effects wear off, perpetuating the cycle of addiction.
Long-Term Consequences of Nicotine Use
- Neuroadaptation and Tolerance: Prolonged exposure to nicotine leads to neuroadaptation, where the brain adjusts to the continued presence of the drug by altering receptor density and sensitivity. This adaptation is a primary driver of tolerance, requiring users to consume more nicotine to achieve the same effects, further embedding the addiction.
- Withdrawal and Dependence: When nicotine use is reduced or stopped, the absence of its stimulatory effects on nAChRs leads to withdrawal symptoms, including irritability, anxiety, difficulty concentrating, and cravings. These symptoms can be severe and make quitting challenging.
- Risk of Neurodegenerative Diseases: Chronic nicotine use is associated with an increased risk of neurodegenerative conditions, such as Parkinson’s disease. Although some studies suggest that nicotine may have neuroprotective properties, the overall impact of chronic exposure, especially through smoking, outweighs these potential benefits due to the presence of other harmful chemicals in tobacco smoke.
Insights from Research: Why Understanding This Mechanism Matters
Research into nicotine’s effects on the brain has profound implications for both treatment and prevention of addiction. For instance, understanding the specific pathways and receptors involved has led to the development of smoking cessation aids like nicotine replacement therapies, varenicline, and bupropion. These treatments work by either mimicking nicotine’s effects in a safer form or by blocking nicotine’s ability to stimulate dopamine release.
Moreover, research continues to explore the therapeutic potential of targeting nAChRs for conditions beyond addiction, such as cognitive disorders. However, such treatments must carefully balance the need to avoid the addictive properties of nicotine while harnessing its beneficial effects.
Conclusion
The brain’s confusion between nicotine and acetylcholine is a key factor in the addictive power of nicotine. By hijacking the acetylcholine receptors, nicotine disrupts normal neurotransmitter function, leading to addiction, cognitive changes, and broad physiological impacts. Understanding this mechanism not only sheds light on the challenges of nicotine addiction but also opens pathways for more effective treatments and interventions. As research advances, a deeper understanding of nicotine’s interaction with acetylcholine receptors could lead to innovative approaches to managing addiction and potentially exploiting these pathways for therapeutic benefits.
References
For an in-depth exploration of nicotine and acetylcholine interactions, readers can refer to studies published in journals such as Nature Neuroscience, The Journal of Neurochemistry, and reports by the National Institute on Drug Abuse (NIDA). These sources provide extensive data and insights into the molecular biology of addiction, the neuroadaptive processes involved, and current trends in treatment approaches.